(June 2022 – August 2023)
Published in Conference: International Society For Quality In Health Care (ISQua)
Authors: Ju-Chun Chien*, Samantha Shih**, Edward Wu**, Louis Tsai**
* Professor at Department of Healthcare Administration, Asia Eastern University of Science and Technology
** Student at Morrison Academy Taichung
Conducted a study to determine the perceived facilitators and barriers of online treatment and identify the principal predictors of online treatment behavioral intention; second author; published paper in International Society for Quality in Health Care(ISQua) 39th International Conference
Abstract
Title
Determining Facilitators and Barriers to Online Treatment Usage for Taiwanese People With and Without Experience
Background
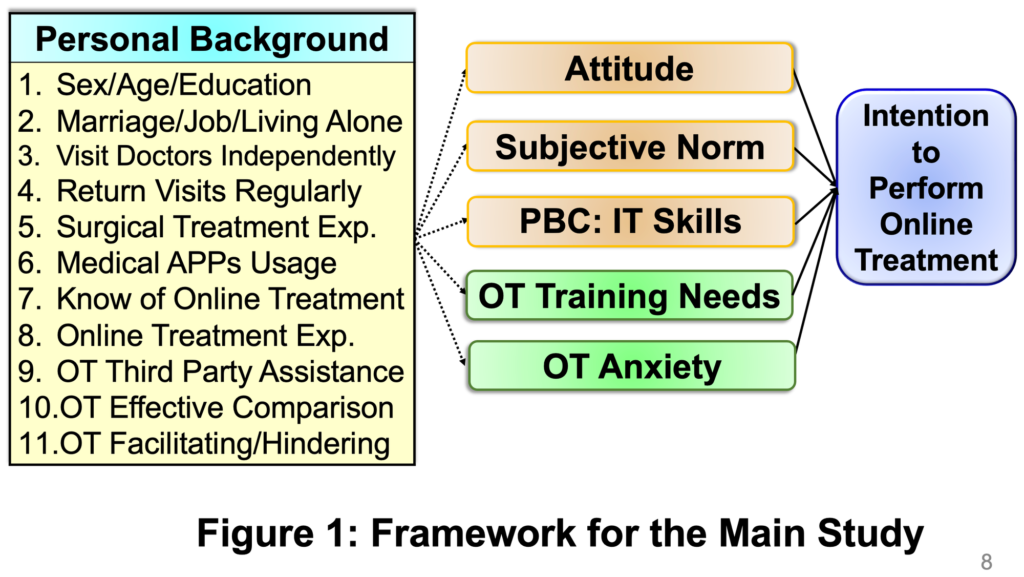
During the COVID-19 pandemic, more people started experiencing online treatment (OT) in Taiwan. OT Anxiety (ANX) and OT Training Needs (TN) were added to the TPB (Theory of Planned Behavior) model to examine factors affecting Taiwanese people’s intention to use OT and the reasons behind them.
Objectives
Determine the perceived facilitators and barriers of OT and identify the principal predictors of OT behavioral intention.
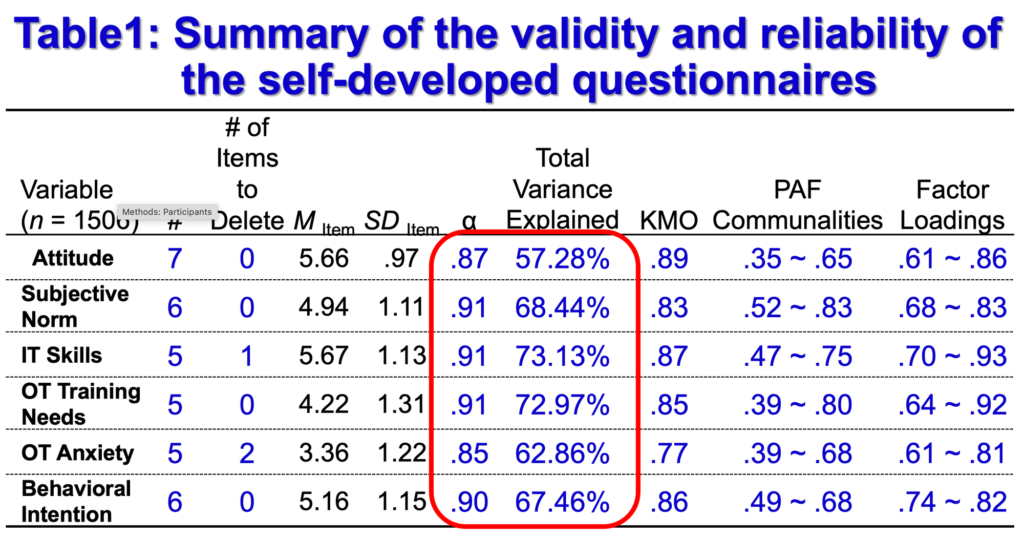
Methods
A pilot study with 426 valid participants was conducted to test the quality and efficiency of the self-developed questionnaire through the 7-point Likert scale. The main study was surveyed online from October 26 to November 26 in 2022, with a total of 1506 valid participants (88.10%) remaining after conducting the reverse wording attention check method. The final research instrument included 9 parts: Personal Background Information (14 items), OT Facilitators (6 statements), OT Barriers (8 statements), Behavioral Intention (BI, 6 items), Attitude (ATT, 7 items), Subjective Norm (SN, 6 items), Perceived Behavior Control: IT skills (ITS, 5 items), OT Training Needs (TN, 5 items), and OT Anxiety (ANX, 5 items). BI, ATT, SN, ITS, TN, and ANX could explain between 57.28% and 73.13% of the total variance. The reliability coefficients were between .87 and .91. Thus the instrument had good psychometric qualities and validity. Descriptive statistics, the EFA, reliability analysis, contingency table analysis, ANOVA, correlation analysis, and multiple stepwise regression were utilized for data analysis.
Results
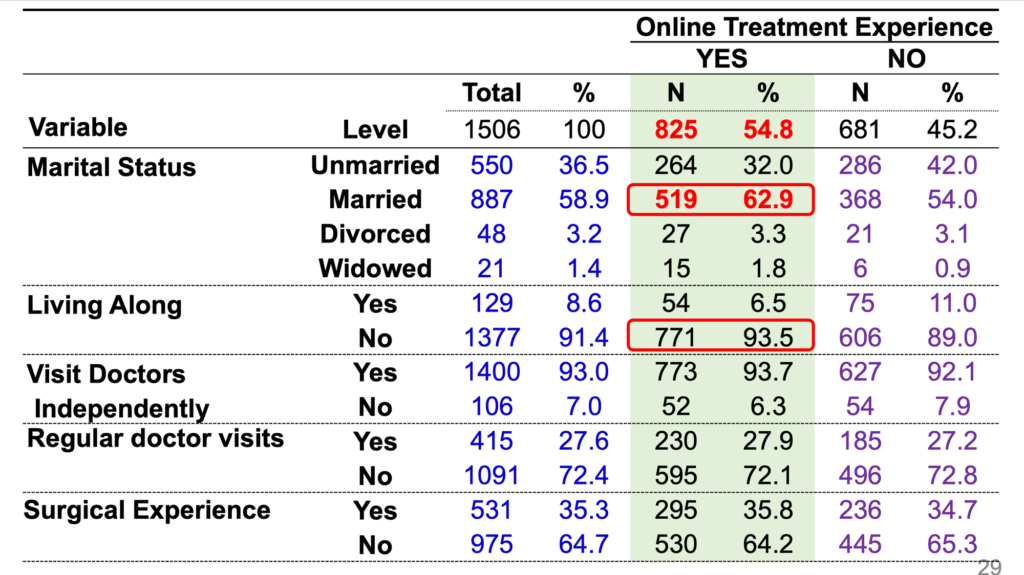
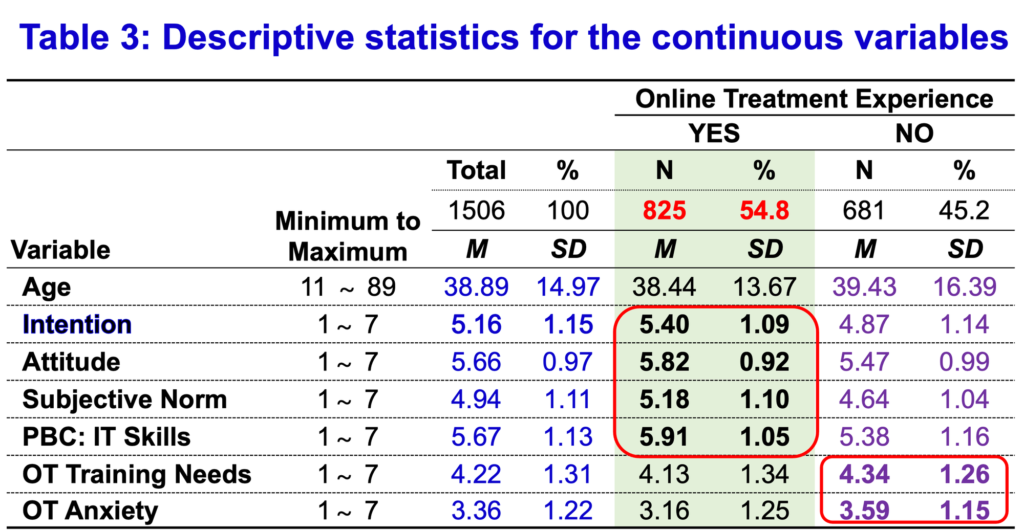
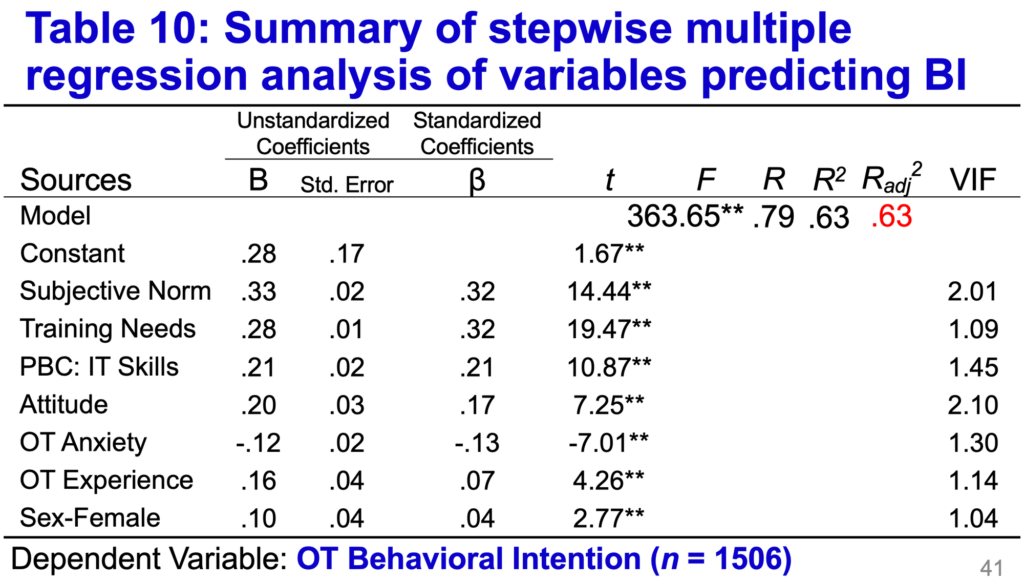
The ages of the 1506 valid participants ranged from 11 to 89 years old (M = 38.89, SD = 14.97); 55% identified as female, 90% knew of OT, and about 55% had OT experience (EXP, n = 825). Most participants showed an acceptance for OT usage (Mitem = 5.16, SDitem = 1.15), with the facilitator being “Unable to attend all doctor visits (n = 636, 42.2%),” and their greatest concern being misdiagnosis (n = 808, 53.7%). Comparing the effects of online treatment and traditional in-person treatment, people with OT experience gave more positive feedback to OT than inexperienced people. For participants with both OT experience and positive feedback to OT, the facilitating factors were infection prevention and saving medical treatment time. Technological and power stability issues were their greatest concern. Participants who were female, had higher education, were employed, and were married showed significantly higher intention to engage in OT. There was a moderate correlation between ATT, SN, ITS, TN, ANX, and BI, respectively. The best predictors of OT intention were SN (β = .32), TN (β =.32), ITS (β =.21), ATT (β =.17), ANX (β = –.13), EXP (β =.07), and Female (β =.04), accounting for 63% of the total variance.
Conclusion
People with OT experience gave positive evaluations for OT, demonstrating the high quality of Taiwanese medical care and the potential for the expansion of OT by the government. As the pandemic was still widely spread in Taiwan, sharing OT experience, mass media promotion, technological and power stability, recording accurate vital signs training courses, and decreasing OT anxiety could facilitate OT usage in Taiwan. Moreover, to prevent the risk of misdiagnosis via OT, patients should be encouraged to ask as many questions as needed. Lastly, the framework of TPB provided a good foundation to understand people’s intention to use OT.
Key Words
Anxiety
Online Treatment
Theory of Planned Behavior
Training Needs
Introduction
Online Treatment, also referred to as telemedicine, was a health-related service by means of information and communication technology (ICT) in order to provide timely medical diagnosis, treatment and monitoring of patients at any location.
The major advantages of online treatment were:
- To deliver treatments for isolated populations (Parmar et al., 2015)
- More convenient (Dorsey et al., 2020)
- Cheaper (Lakshin et al., 2021; Wootton, 2001)
- To spare the time (Caponnetto et al., 2022)
- To prevent infection (Kapoor et al., 2020)
Some disadvantages of online treatment were:
- Inability to perform full physical examination (Stifani et al., 2021)
- To increase potential diagnostic errors (Wang et al., 2023)
- The digital divide (Kichloo et al., 2020)
- People with poor technological literacy (Florea et al., 2021)
- Increased security concerns (Mills et al., 2020)
Despite the above limitations, in general, patients consistently reported a high level of satisfaction with telemedicine-based care (Alsabeeha et al., 2023; Lakshin et al., 2021; Nie et al., 2022; Parmar et al., 2015; Pogorzelska & Chlabicz, 2022; Yoon et al., 2021). In addition, online treatment usage increased rapidly during the COVID-19 pandemic (Nittari et al., 2022).
In 2020, the Institute for Healthcare Improvement developed a framework for ensuring safe, equitable, person-centered telemedicine (Perry et al., 2021). The six elements were:
- Access: Overcome infrastructure and technological barriers
- Privacy: Manage cybersecurity risk
- Diagnostic Accuracy: Reduce diagnostic errors
- Communication: Offer training to providers and patients to diminish technical, emotional, and psychological communication challenges
- Psychological and Emotional Safety: Be mutually reinforcing between patients and providers
- Human Factors and System Design: Be fully integrated into the existing system and apply user-centered co-design
In other words, to successful implementation of online treatment, patients’ psychological concerns, IT skills, and related trainings were addressed. Moreover, one of the factors that influenced online treatment adoption was digital literacy (Lopez et al., 2021). In addition, anxiety to technology was related to willingness to use telepsychiatry (Werner, 2004). On the other hand, the Theory of Planned Behavior Model could explain 85.8% of the intention to use telemedicine (Ramírez-Correa et al., 2020).
Taiwan’s National Health Insurance (NHI) System has implemented for 20 years. It has provided most convenient healthcare possible. However, according to National Health Insurance Administration (NHIA), even during the COVID-19 pandemic, about 33,000 Taiwanese people still sought medical treatment (doctor shopping) more than 90 times per person in 2020. On the other hand, there was still room for improvement in Taiwanese people’s awareness and needs for telemedicine in 2020 (Chang et al., 2021). Facing the COVID-19 outbreak and related lockdown, from May 2021, NHIA expanded telemedicine services to all citizens. Therefore, more and more people started experiencing online treatment in Taiwan.
This study was conducted in 2022. In addition to exploring the reasons and concerns about online treatment usage between Taiwanese people with and without the experience, by means of the extended Theory of Planned Behavior (TPB) model, the present study also examining principal predictors of online treatment behavioral intention.
Objectives
- Understand the proportion of observations in the sample that have actual experience of online treatment and to reveal participants’ perceived benefits and barriers about the use of online treatment.
- Examine the differential effects of personal background information on online treatment behavioral intention.
- Analyze the differences between experienced and inexperienced OT individuals in the background variables and the main dependent variables.
- Investigate the correlation between the main continuous variables to OT behavioral intention.
- Identify the important predictors of OT behavioral intention.
Method
Participants
A pilot study with 426 valid participants was conducted to test the quality and efficiency of the self-developed online questionnaire through the 7-point Likert scale.
The main study was surveyed online from October 26 to November 26 in 2022. The data were gathered using convenience sampling, with a total of 1506 valid participants (88.10%) remaining after conducting the reverse wording attention check method.
Instrument
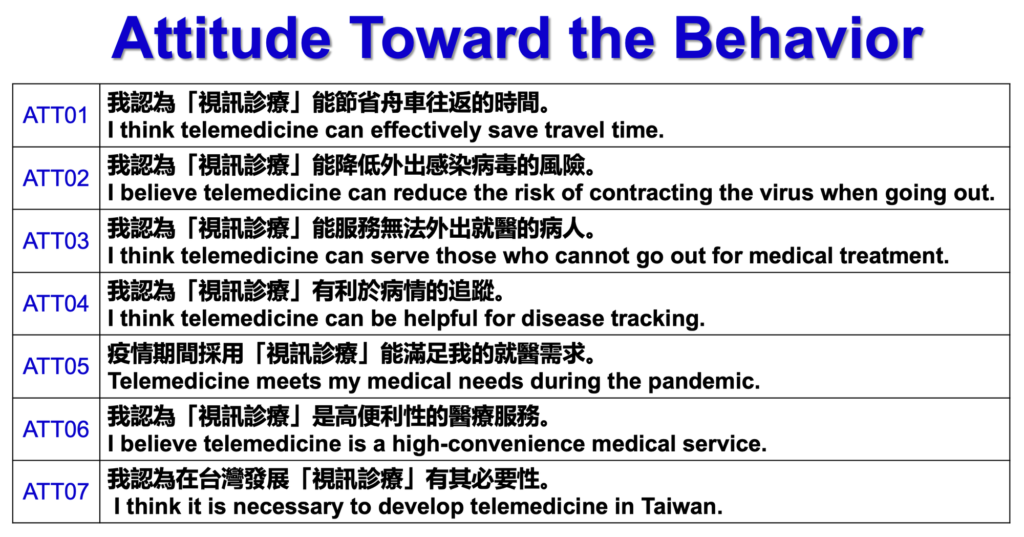
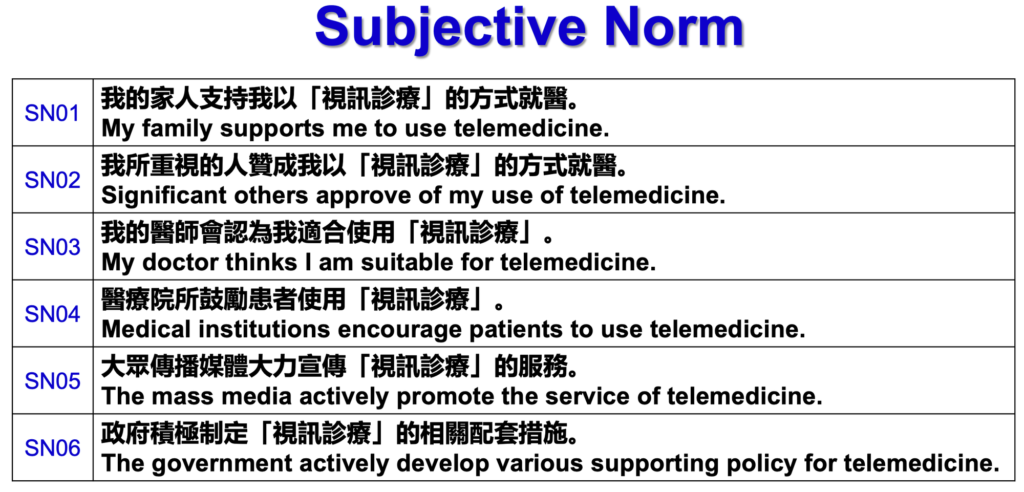
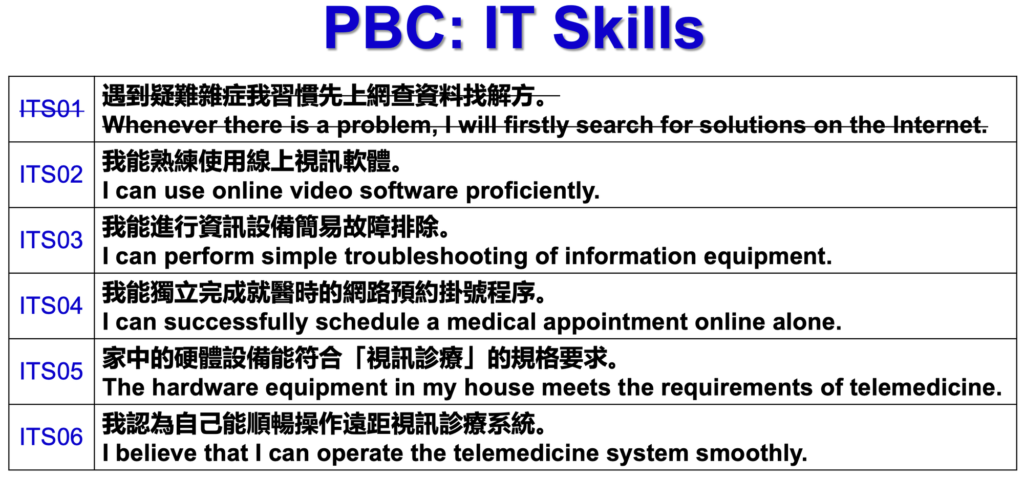
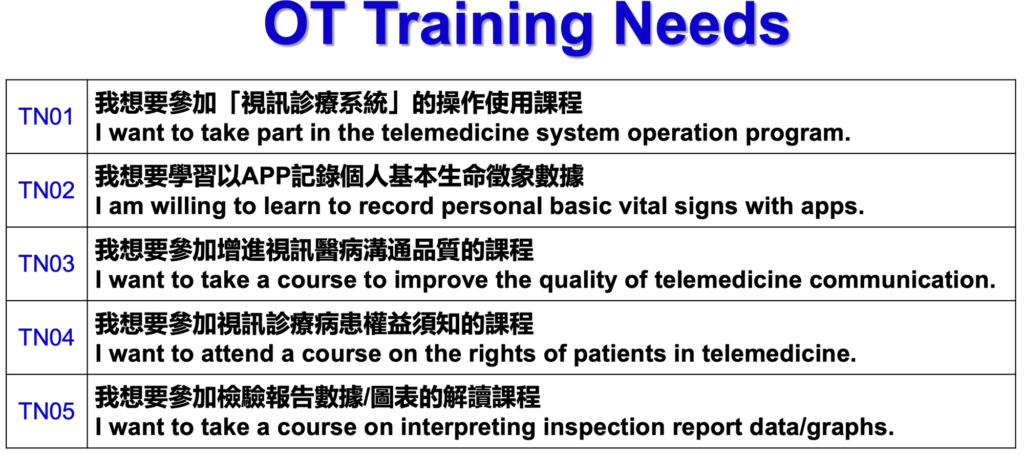
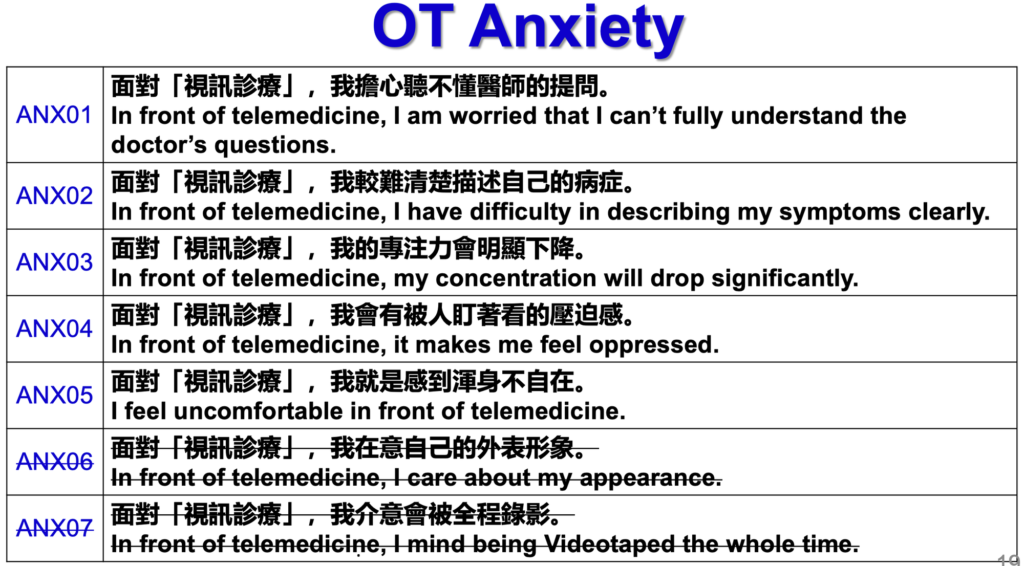
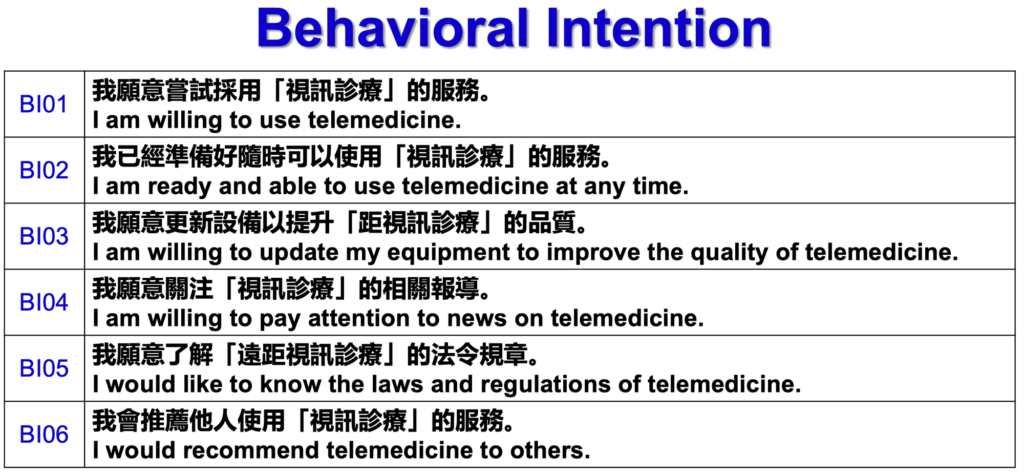
The final research instrument contained 9 parts: Personal background information (14 items), OT benefits (6 statements), and OT barriers (8 statements). Moreover, behavioral intention (BI, 6 items), Attitude (ATT, 7 items), Subjective Norm (SN, 6 items), PBC: IT skills (ITS, 5 items), Training Needs (TN, 5 items), and OT Anxiety (ANX, 5 items)
After conducting the attention check, the EFA, and the internal consistency tests, the final self-developed online questionnaire on a seven-point Likert scale had good construct validity (total variance explained from 57.28% to 73.13%) and reliability (Cronbach’s alpha from .87 to .91).
Term Definitions
- Attitude Toward the Behavior (ATT) – Online treatment is positively or negatively valued by the person. The higher the average score, the more positive an individual’s attitude toward online treatment.
- Subjective Norm (SN) – The degree to which a person perceived significant others believed they should use or not to use online treatment. The higher the mean score meant the more social support the person perceived**.**
- Perceived Behavioral Control: IT Skills (PBC: ITS) – The degree to which a person’s perception of his or her IT ability to perform online treatment. The higher the mean score, the more the person believed that his or her IT skills were sufficient to perform online treatment.
- Online Treatment Training Needs (OT_TN) – A person’s willingness to enhance knowledge and skills in online treatment through training. The higher the mean score, the more the person considered the necessity of acquiring further knowledge on online treatment.
- Online Treatment Anxiety (OT_ANX) – The degree to which a person’s perception of his or her anxiety in front of online treatment. The higher the mean score, the more the person felt uncomfortable and worry about online treatment usage.
- Online Treatment Behavioral Intention (OT_BI) – A person’s readiness to engage in online treatment. The higher the mean score, the stronger the online treatment usage intention.
Survey Questions
Statistical Analysis
Descriptive statistics, exploratory factor analysis (EFA), reliability analysis, contingency table analysis, ANOVA, correlation analysis, and multiple stepwise regression were utilized for data analysis.
Results
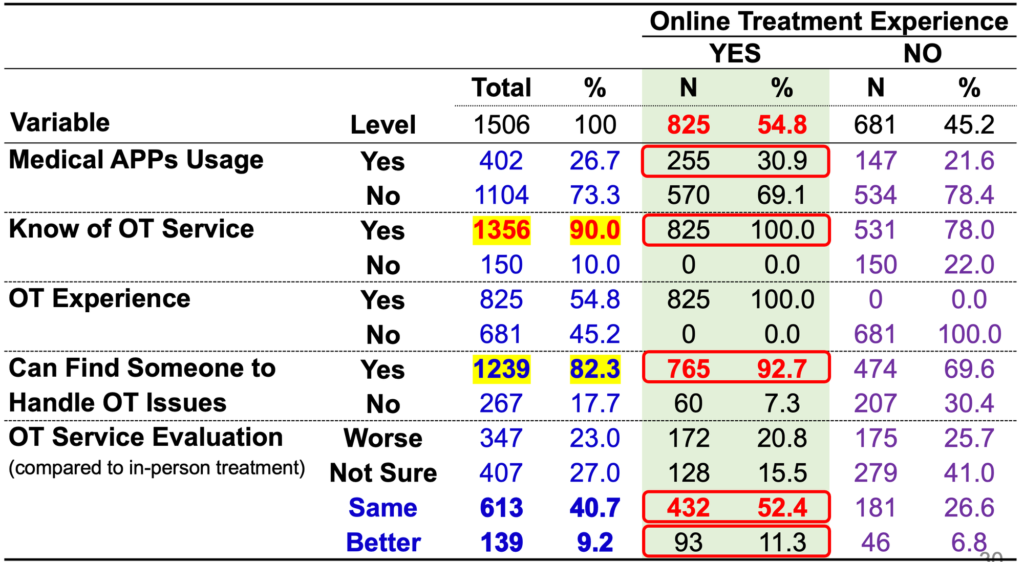
- Ninety percent of the participants (n = 1356) knew of online treatment service; moreover, they displayed a positive intention to use online treatment (5.16 ± 1.15). The majority of people could find someone to handle online treatment issues (n = 1239, 82.3%), and about 55% of the participants had online treatment experience (n = 825). About half of participants (n = 752, 49.9%) considered online treatment was as effective as or better than in-person treatment.
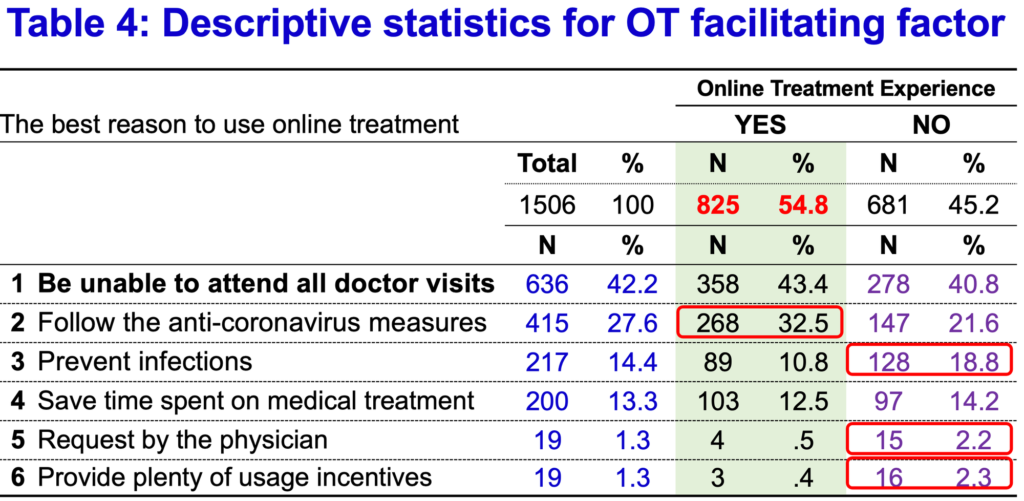
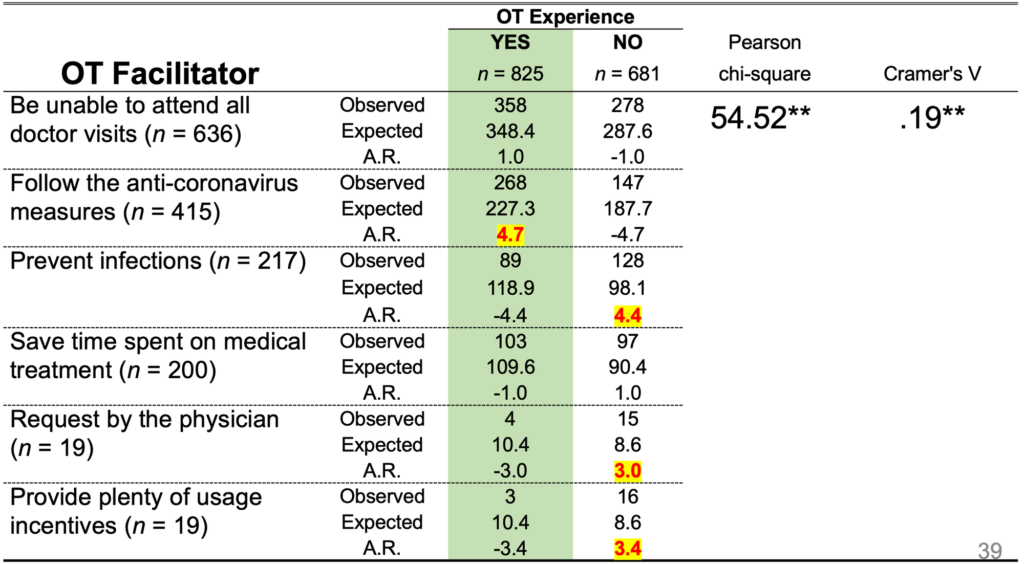
- The three most facilitators for online treatment usage were: (1) Be unable to attend all doctor visits (n = 636, 42.2%), (2) Follow the anti-coronavirus measures (n = 415, 27.6%), and (3) Prevent infections (n = 217, 14.4%).
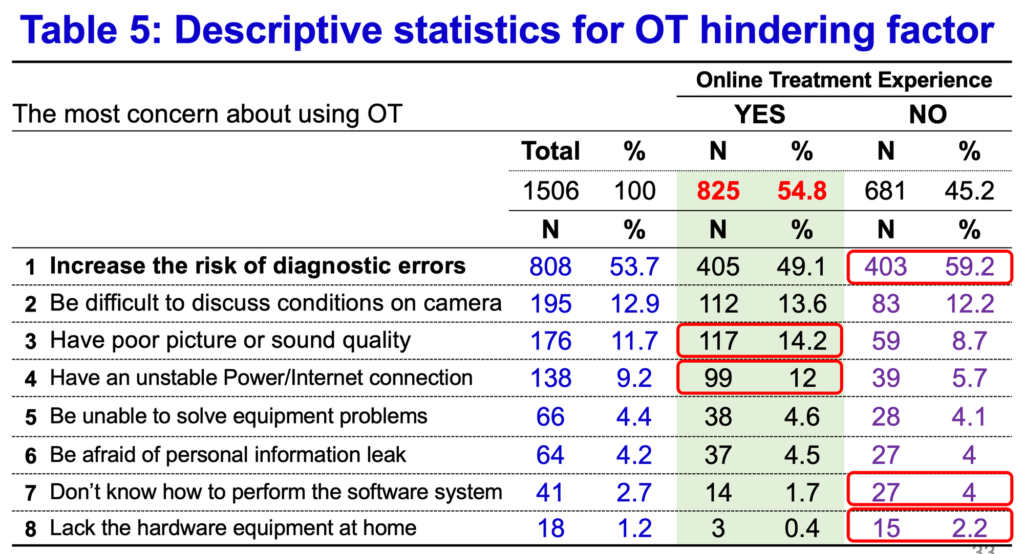
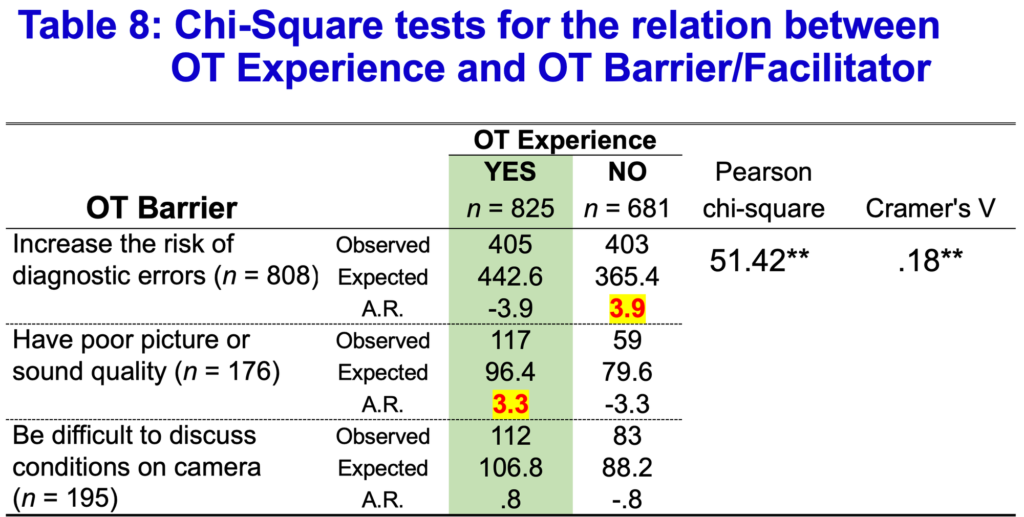
- The three most concerns for online treatment usage were: (1) Increase the risk of diagnostic errors (n = 808, 53.7%), (2) Be difficult to discuss conditions on camera (n = 195, 12.9%), and (3) Have poor picture or sound quality (n = 176, 11.7%).
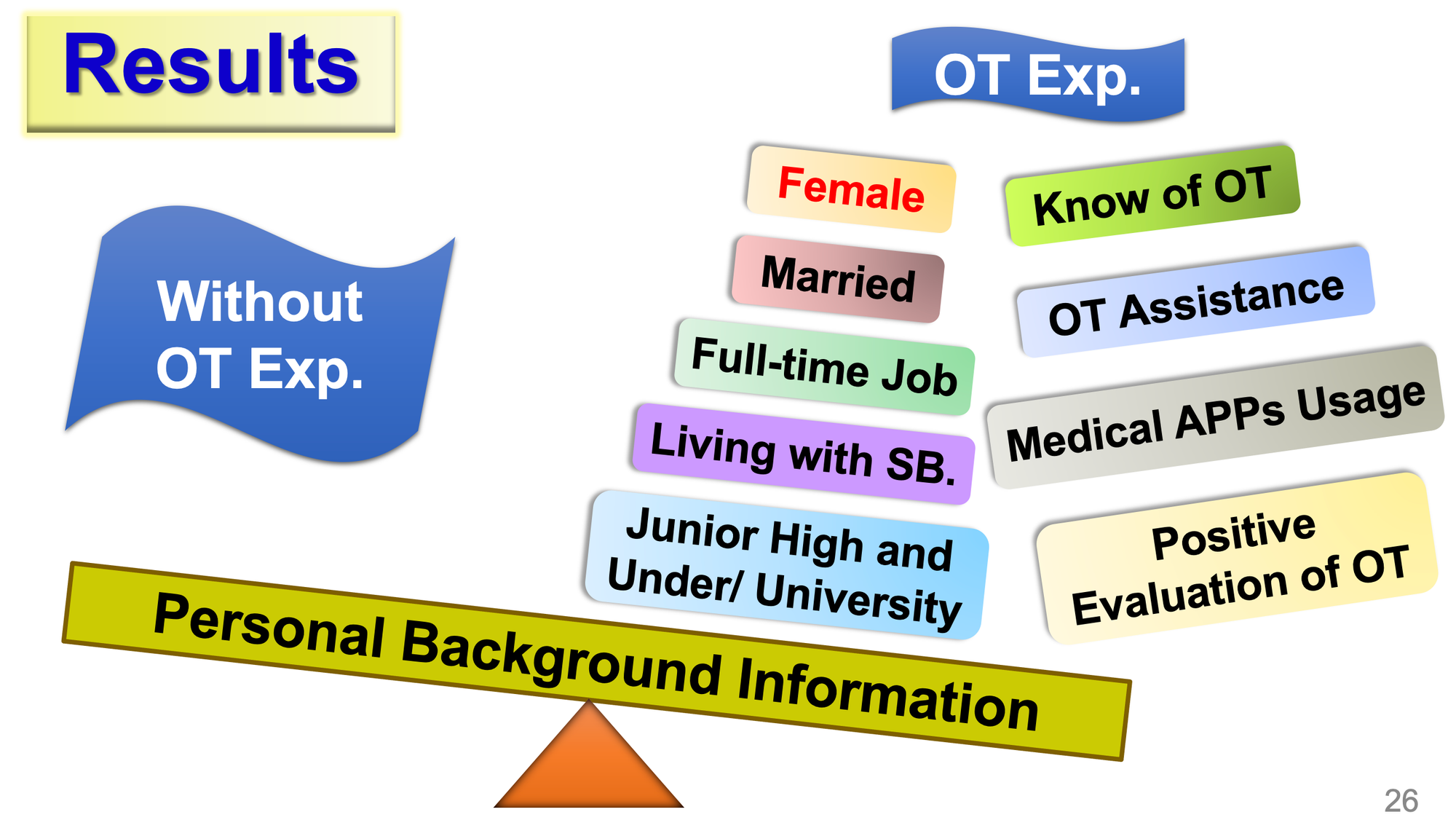
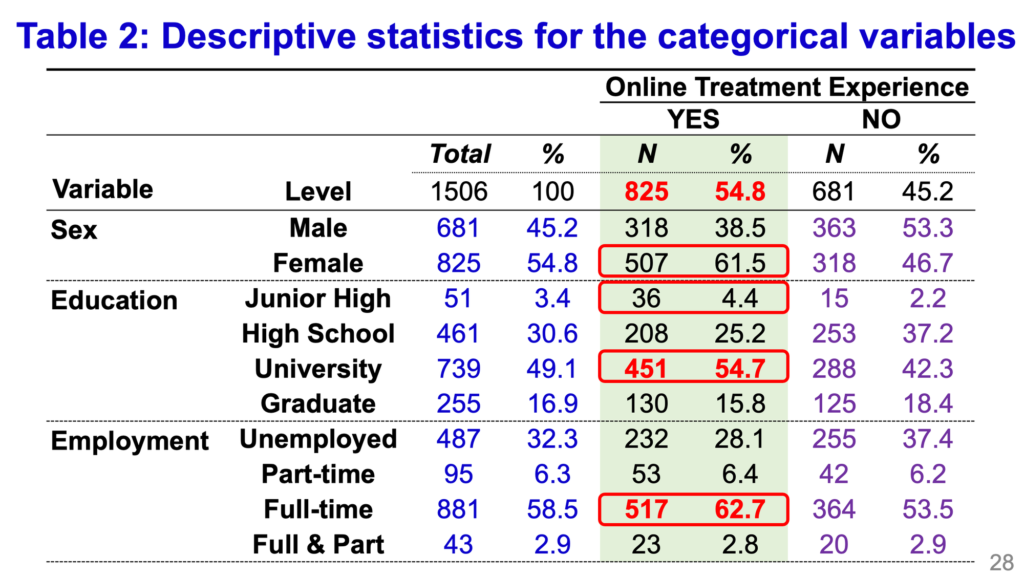
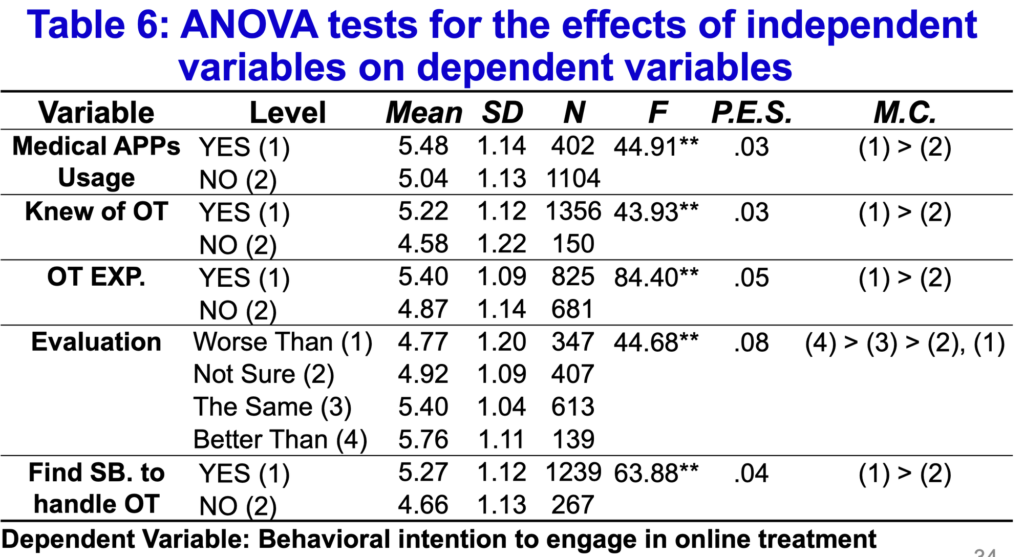
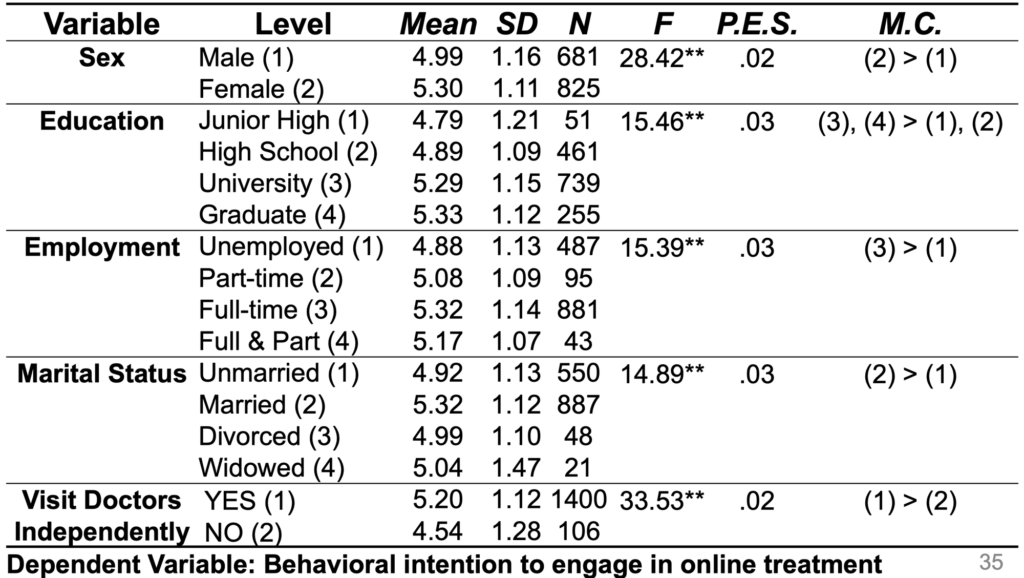
- Participants who were female, had higher education, had full-time job, were married, and could visit doctors independently showed significantly higher intention to engage in online treatment, respectively. In addition, participants who knew of online treatment service, had OT experience, used medical APPs, could find someone to handle OT issues, had positive OT service evaluation reported significantly higher levels of intention to adopt OT, respectively.
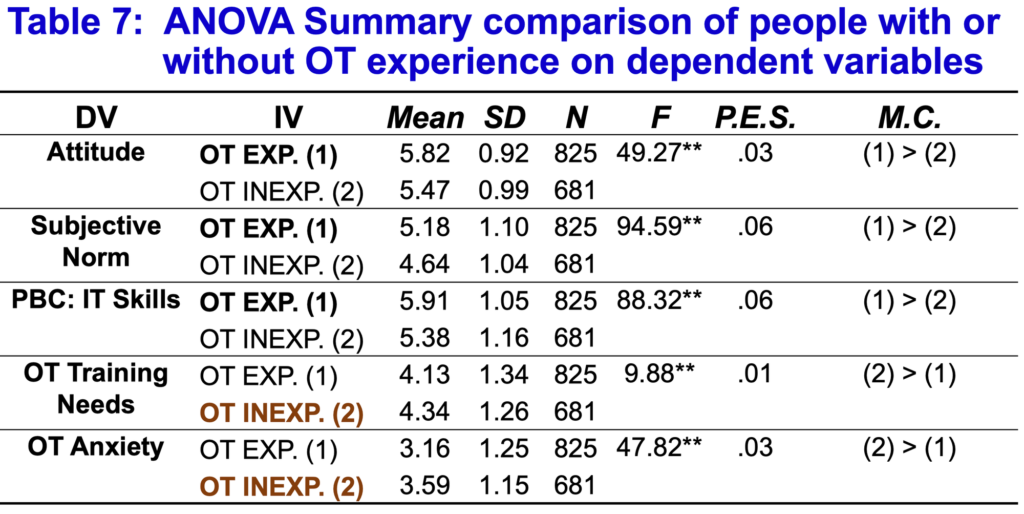
- Compared to people without online treatment experience, those with OT experience revealed significant higher scores in Behavioral Intention, Attitude, Subjective Norm, PBC: IT Skills, respectively. In addition, people without OT experience reported a significant higher score on OT Training Needs and OT Anxiety, respectively.
- Compared to people without online treatment experience, there was a significant amount of people with OT experience chose “Follow the anti-coronavirus measures” as their main reason. On the other hand, a greater proportion of people without OT experience chose “Prevent infections,” “Request by the physician,” and “Provide plenty of usage incentives” as their main reason to use OT.
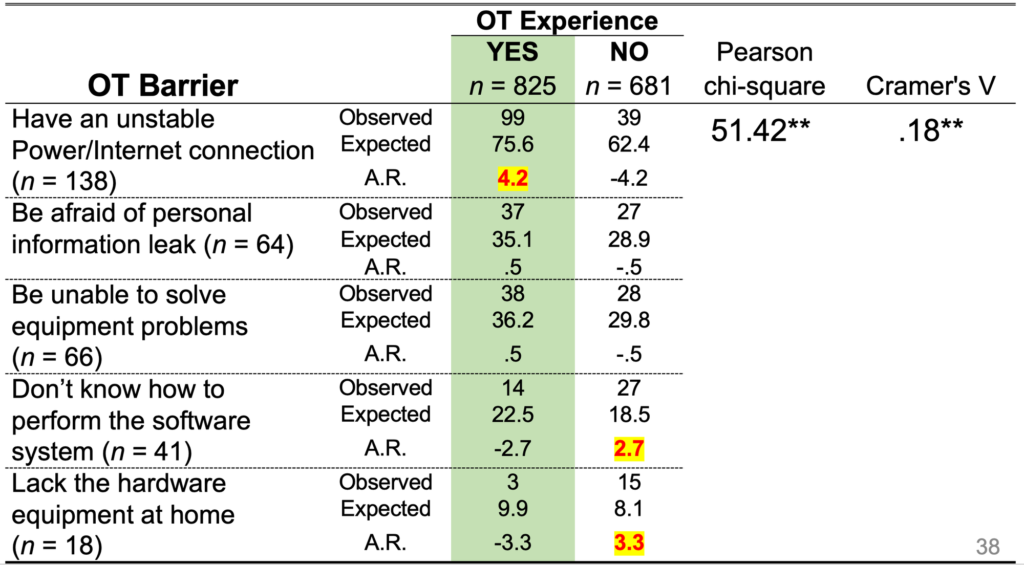
- Compared to people without online treatment experience, there was a significant amount of people with OT experience chose “Have poor picture or sound quality” and “Have an unstable Power/Internet connection” as their main concern. On the other hand, a greater proportion of people without OT experience chose “Increase the risk of diagnostic errors,” “Don’t know how to perform the software system,” and “Lack the hardware equipment at home” as their main concern to use OT.
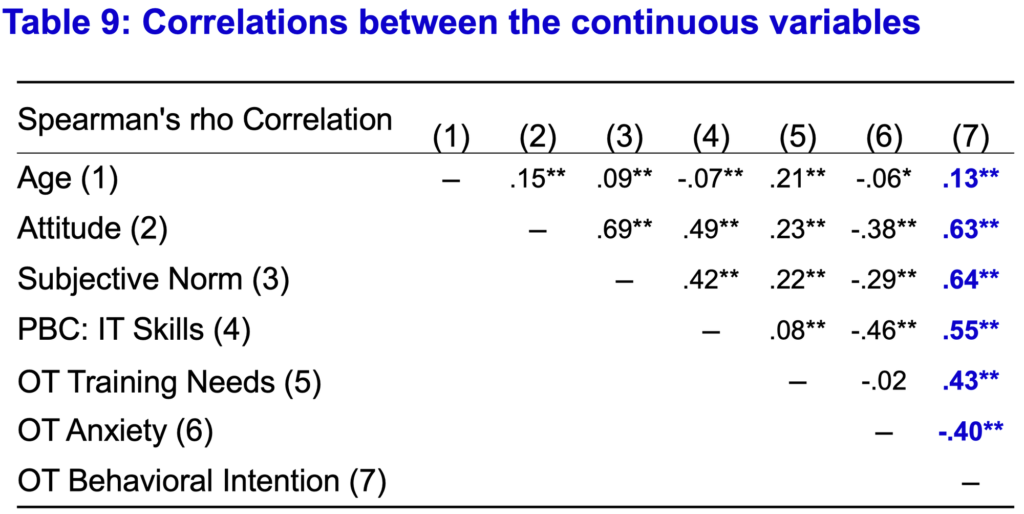
- There was a moderate correlation (from .40** to .64**) between Attitude, Subjective Norm, PBC: IT Skills, OT Training Needs, OT Anxiety, and OT Behavioral Intention, respectively. More specifically, OT Anxiety was negatively correlated (–.40**) with OT Behavioral Intention.
- The best predictors to influence online treatment intention were Subjective Norm (β = .32), OT Training Needs (β =.32), PBC: IT Skills (β =.21), Attitude (β =.17), OT Anxiety (β = –.13), OT Experience (β =.07), and Female (β =.04). These predictors accounted for 63% of the total variance. The regression equation~ BI = .28 + .33X1 +.28X2 +.21X3 +.20X4 – .12X5 + .16X6 +.10X7
Conclusion
- More than half of respondents had actual online treatment experience in this study indicated that the COVID-19 pandemic and mobility restrictions put a spotlight on online treatment as an alternative method to provide medical services and to reduce the risk of infection in Taiwan.
- Even though people displayed a positive intention to use online treatment and about half considered online treatment was as effective as or better than in-person treatment, the greatest concern for using online treatment was the risk of being misdiagnosed.
- The Theory of Planned Behavior was an effective model for predicting people’s intention to use online treatment; besides, OT Training Needs, OT Anxiety, and OT experience had significant impacts on online treatment usage intention.
- People with online treatment experience not only revealed different reasons and concerns about the use of online treatment than those inexperienced, but also gave a positive evaluation for the quality of online treatment. The results supported the high quality of Taiwanese medical care and the potential for the expansion of online treatment in the future.
Significance
- This study used a sufficient sample to compare the differences between those with and without online treatment experience, the results could be used as a more detailed reference for the government to establish epidemic prevention policies and strategies.
- The self-developed questionnaire had rigorous construct validity and reliability, it could be used as a valuable reference for subsequent related studies.
Limitations
- This study was based on the respondents’ recall of online treatment usage, the possibility of memory distortion might not be ruled out.
Conference Pictures from ISQua






References
Alsabeeha, N. H., Atieh, M. A., & Balakrishnan, M. S. (2023). Older adults’ satisfaction with telemedicine during the COVID-19 pandemic: a systematic review. Telemedicine and e-Health, 29(1), 38-49. Caponnetto, V., Ornello, R., De Matteis, E., Papavero, S. C., Fracasso, A., Di Vito, G., … & Sacco, S. (2022). The COVID-19 pandemic as an opportunity to improve health care through a nurse-coordinated multidisciplinary model in a headache specialist center: the implementation of a telemedicine protocol. Telemedicine and e-Health, 28(7), 1016-1022. Chang, E., Chao, C., Yeh, W., Lin, H., & Chang, S. (2021). ‘Research on needs for the telehealth service due to Covid-19’, Taiwan Medical Alliance Academic Journal, (1), 27-60. Dorsey, E., Okun, M. S., & Bloem, B. R. (2020). Care, convenience, comfort, confidentiality, and contagion: the 5 C’s that will shape the future of telemedicine. Journal of Parkinson’s disease, 10(3), 893-897. Florea, M., Lazea, C., Gaga, R., Sur, G., Lotrean, L., Puia, A., … & Sur, M. L. (2021). Lights and shadows of the perception of the use of telemedicine by romanian family doctors during the COVID-19 pandemic. International Journal of General Medicine, 1575-1587. Hjelm, N. M. (2005). Benefits and drawbacks of telemedicine. Journal of telemedicine and telecare, 11(2), 60-70. Kapoor, A., Guha, S., Das, M. K., Goswami, K. C., & Yadav, R. (2020). Digital healthcare: The only solution for better healthcare during COVID-19 pandemic?. Indian Heart Journal, 72(2), 61-64. Kichloo, A., Albosta, M., Dettloff, K., Wani, F., El-Amir, Z., Singh, J., … & Chugh, S. (2020). Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Family medicine and community health, 8(3). Lakshin, G., Banek, S., Keese, D., Rolle, U., & Schmedding, A. (2021). Telemedicine in the pediatric surgery in Germany during the COVID-19 pandemic. Pediatric Surgery International, 37, 389-395. Lopez, A. M., Lam, K., & Thota, R. (2021). Barriers and facilitators to telemedicine: can you hear me now?. American Society of Clinical Oncology Educational Book, 41, 25-36. Mills, E. C., Savage, E., Lieder, J., & Chiu, E. S. (2020). Telemedicine and the COVID-19 pandemic: are we ready to go live?. Advances in skin & wound care. Nie, J. Z., Karras, C. L., Texakalidis, P., Trybula, S. J., & Dahdaleh, N. S. (2022). A systematic review on outpatient telemedicine utilization in neurosurgery following the start of COVID-19. World Neurosurgery. Nittari, G., Savva, D., Tomassoni, D., Tayebati, S. K., & Amenta, F. (2022). Telemedicine in the COVID-19 era: a narrative review based on current evidence. International Journal of Environmental Research and Public Health, 19(9), 5101. Perry AF, Federico F, Huebner J. Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care. IHI White Paper. Boston: Institute for Healthcare Improvement; 2021. (Available at www.ihi.org) Pogorzelska, K., & Chlabicz, S. (2022). Patient satisfaction with telemedicine during the COVID-19 pandemic—a systematic review. International Journal of Environmental Research and Public Health, 19(10), 6113. Ramírez-Correa, P., Ramírez-Rivas, C., Alfaro-Pérez, J., & Melo-Mariano, A. (2020). Telemedicine acceptance during the COVID-19 pandemic: an empirical example of robust consistent partial least squares path modeling. Symmetry, 12(10), 1593. Stifani, B. M., Avila, K., & Levi, E. E. (2021). Telemedicine for contraceptive counseling: An exploratory survey of US family planning providers following rapid adoption of services during the COVID-19 pandemic. Contraception, 103(3), 157-162. Wang, J. J., Zhang, X., & Shi, J. J. (2023). Hospital dual-channel adoption decisions with telemedicine referral and misdiagnosis. Omega, 119, 102875. Werner, P. (2004). Willingness to use telemedicine for psychiatric care. Telemedicine Journal & e-Health, 10(3), 286-293. Wootton, R. (2001). Telemedicine. British Medical Journal, 323(7312), 557-560. Yoon, E. J., Tong, D., Anton, G. M., Jasinski, J. M., Claus, C. F., Soo, T. M., & Kelkar, P. S. (2021). Patient satisfaction with neurosurgery telemedicine visits during the coronavirus disease 2019 pandemic: a prospective cohort study. World Neurosurgery, 145, e184-e191.